Inching back to Normal: Tradeoffs between transmission rates and herd immunity
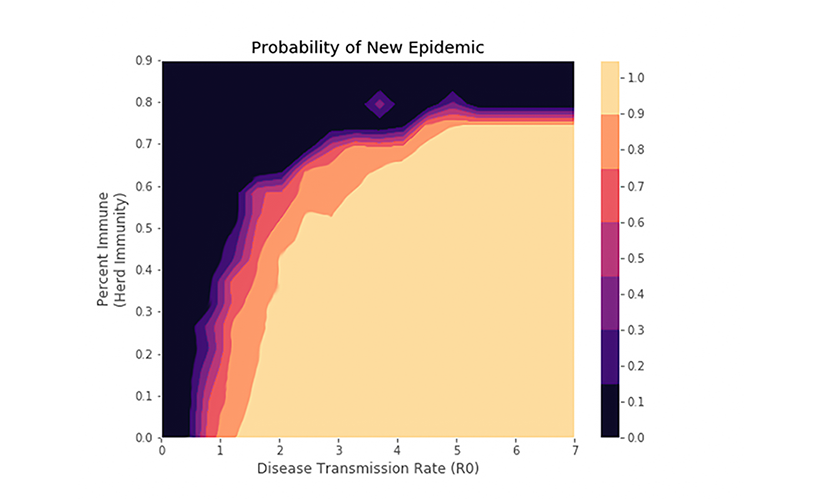
As MIT and the country fight to limit the effects of the COVID-19 pandemic, one question yet to be answered is how and when we should return to our normal lives. While there are many aspects that can impact policy choice, the percentage of the community that is immune ought to play an important role. In particular, it is very useful to know the tradeoff between immunity and transmission rate to prevent reinfection. Using a network model we have developed, we find how the probability of a new infection becoming an epidemic varies as a function of the level of immunity and connectivity (see the plot below). Our results indicate that once a certain proportion of the population is immune to the virus — commonly called herd immunity — the probability that an epidemic will emerge is extremely low even with minimal social distancing imposed.
Our simulation uses an underlying network to model the transmission of the virus and its outcomes through a population. The virus spreads probabilistically at each time step through connections described by the network. Depending on their age, once an individual contracts the disease they will experience a set of outcomes (e.g. hospitalization, ICU, death, or recovery). The probability of each of these outcomes occurring was calibrated using data from the CDC. Using this model, we seek to understand how the underlying network structure impacts the progression of the disease.
In particular, the effects of both the transmission rate of the virus (which can be controlled through methods like social distancing) and the level of herd immunity, modify the probability of a new epidemic spreading through the population. We can see that below a herd immunity of 40% the probability of a new epidemic uniformly increases linearly with transmission rate, indicating that any immunity level below 40% is unlikely to effect the trajectory of future disease spread. On the other had, a herd immunity level above 70% percent appears to limit the spread of new infections regardless of transmission rate. As we think about policy for re-opening society, we should carefully assess the level of herd immunity and use it to decide level of interventional policy.
At a practical level, we hope to use our model to test different strategies to allow MIT to reopen. How much testing would be necessary to contain future outbreaks if MIT employed some kind of contact tracing? Does this parameter depend on the proportion of the original population that had immunity to the virus? If there were a phased reintroduction of students and faculty to MIT, who should come back first and when? These are some of the questions we seek to answer with our model.
For further details, please contact Dalton Jones or Munther Dahleh.